HEALTHCARE PROFESSIONALS
How IOPI can help your patients
What It Does and How It Helps
The Iowa Oral Performance Instrument (IOPI) objectively measures:
- tongue strength and endurance
- lip strength and endurance
- objectively documenting deficits that justify treatment
- diagnostically differentiating between muscle weakness and problems of motor control
- providing biofeedback during isometric oral motor exercise programs
- motivating patients by showing them their progress from muscle exercise therapy

HOW IT WORKS
Measures Strength
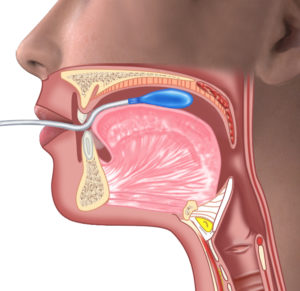
The IOPI measures the strength of the tongue by measuring the maximum pressure that an individual can produce in a standard-sized air-filled bulb by pressing the bulb against the roof of the mouth with the tongue. The peak pressure achieved is displayed on a large, easy-to-read LCD. The units displayed are kilopascals (kPa), based on the internationally-recognized unit of pressure, the Pascal (Pa).
Lip compression strength depends on the strength of the circumferential muscle complex that surrounds the mouth. It is the tension in these muscles that allows the lips to be compressed against one another. The bulb, placed under the lips at the corner of the mouth, measures the maximum pressure created when a patient presses their lips together and “purses” as hard as they can.
Exercise Therapy
The IOPI has a vertical row of lights (LEDs) on the front of the instrument. The higher the pressure, the higher the position of the light that is turned on. Producing a pressure that can turn on the top (green) light can be thought of as “winning” (“I hit the target!”). The pressure required to illuminate the green light at the top of the IOPI’s light array can be adjusted using the Set Max arrow buttons. The healthcare professional determines what target value is appropriate for exercise therapy purposes and provides specific instructions to the patient for a particular exercise protocol. A protocol should include the target value to set, the number of times to illuminate the green light and, for each repetition, how long the green light should be illuminated before releasing pressure on the bulb.
T= Target value, Pmax = maximum tongue pressure, E = Effort (%)
Posterior Tongue Elevation
Measures Endurance
In patients with dysphagia or dysarthria, oral motor fatigability may be of interest. The IOPI can be used to assess tongue fatigability by measuring its endurance, which is inversely proportional to fatigability. Low endurance values are an indicator of a high fatigability.
Endurance is measured with the IOPI by quantifying the length of time that a patient can maintain 50% of his or her maximum pressure. This procedure is conducted by setting the target value in the Target Mode to 50% of the patient’s maximum pressure and timing how long the patient can hold the top (green) light on.
VALIDATION
The IOPI® has been validated in many scientific studies, and normal standards exist for tongue elevation strength.
TONGUE STRENGTH
Clinical Importance
Knowing a patient’s tongue strength is clinically useful for several reasons:
- DECIDING whether tongue weakness is involved in oral stage swallowing problems and/or dysarthria:
- If the tongue is weak, you can start tongue strengthening therapy.
- If the tongue strength is normal, you can eliminate weakness as a cause of the swallowing or speech problems, and thus concentrate on other more useful therapies.
- DOCUMENTING that a patient’s tongue is weak, and therefore that strengthening exercises are justified. This may be important to insurance providers and administrators who are concerned with the cost of delivering such therapy.
- ASSESSING the results of tongue strengthening therapy over time:
- If tongue strength doesn’t increase over time, then perhaps the patient is not performing the prescribed exercises, or not doing them forcefully enough.
- If the tongue strength does increase, even a little bit, it can be "rewarding" for the patient to see concrete evidence improvement.
- EXERCISING the patient’s tongue. Performing tongue exercise using an IOPI® can give the patient very specific "targets" to achieve with their efforts, and give them immediate feedback about improvement.
Posterior Tongue Elevation
Slide arrows to see before and after
Tongue Exercise using BIOFEEDBACK
Evidence exists to show that tongue exercise in dysphagia patients, as documented with the IOPI, can lead to improved swallowing outcomes. The IOPI allows the clinician to use protocols that have been proven to work in exercise science. The clinician sets the target pressure on the IOPI’s biofeedback light array and instructs the patient to squeeze the bulb until they turn the top green light on. The patient is visually reinforced for hitting their target.
Anterior Tongue Elevation
Pressure as a Measure of Strength
Tongue Elevation Strength
- Repeated measurements of tongue strength in the same individual are quite reliable, particularly after the patient has done the task a few times.
- There is considerable variability in tongue strength in a population of adults reporting no swallowing or speech problems (see Normal Values). There is a clear central tendency, however, with an average maximum pressure of about 60 kPa, and a range of 40-80 kPa.
- Patients with oral phase swallowing problems have a tongue strength that is significantly lower than the normal population.
LIP STRENGTH
Why Measure Lip Strength?
Inadequate lip strength may contribute to problems with deglutition, such as food containment during chewing. If lip weakness is severe, it also may interfere with the production of plosive speech sounds. Such weakness would probably be obvious, but being able to accurately "track" the degree of weakness would enable the clinician to determine whether the weakness is getting better or worse, and/or determine if training improves lip strength. Additionally, observing lip weakness in a patient may help identify abnormalities within the nervous system such as subtle cortical dysfunction, or disease processes gradually affecting the function of the facial nerve.
Lip Strength Measurement
To measure lip strength, an IOPI bulb is placed inside the cheek just lateral to the corner of the mouth and the patient squeezes the IOPI bulb against the buccal surface of the teeth by pursing the lips as hard as possible. Although the bulb is not directly between the lips, it is valid because the pressure developed in the bulb depends upon the strength of the circumferential muscle complex that surrounds the mouth, in particular the obicularis oris. It is tension in these muscles that allows the lips to be compressed against one another.
Asymmetrical lip strength may reveal neurological problems of the brain or peripheral nerves.
Food containment problems, as frequently seen in Traumatic Brain Injury (TBI) patients, can result from lip weakness.